“The time for action is now. It's never too late to do something.”
Antoine de Saint-Exupery
"CURE"
INFORMATION LETTER
Project Founder: Dr. Serguei Kisselev
Editor: Svetlana Kisseleva
Objectives of the “Cure” method
- To promote research into, and knowledge of, the causes, mechanisms, diagnosis, treatment and other aspects of the “Cure” method.
- To provide a forum for the exchange of ideas related to the “Cure” method.
- To educate physicians, other health professionals and the general public about the “Cure” method
- To encourage the management of acute and chronic conditions to be conducted in a scientific and ethical manner.
- To promote, arrange and conduct meetings, seminars, conferences lectures, discussions and courses of study on the “Cure” method and related topics.
Content:
- Age is just a number after all
- Prescribing and dosing exercise in primary care
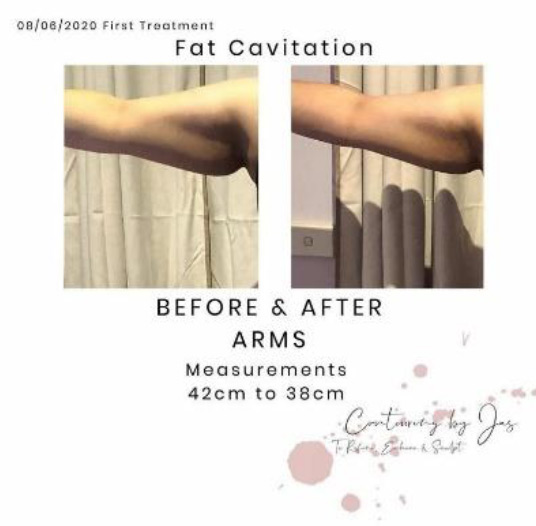
- Fat Cavitation and Skin Tightening as part of the weight management problem
- Case Study
- Australian study finds resistance training improves cognitive function in older adults
- Physiotherapy and the gym
- Would you like to be a part of the CURE Method?
Age is just a number after all.
Ten years of the Sheffield Medical Centre’s Rehabilitation Gymnasium
Svetlana Kisseleva, Editor
It is a common occurrence to hear the words “I’m too old, I can’t go to the gym”. It is even rarer to see anyone over the age of 65 with various chronic conditions to be participating in any rigorous form of physical activity. Despite many studies proving the effectiveness of physical activity for all ages, it seems that any form of gym or fitness centre is populated by the young and the fit. Enter Sheffield Medical Centre’s Rehabilitation Gym.
Celebrating its 10th year at Sheffield Medical centre, the Rehabilitation gym is a vibrant, active, and unique space for people over the age of 65 to participate in an active lifestyle once thought impossible for their age. With trained staff assisting on-site at all opening hours and doctors in the vicinity, this gym is like no other.
Modern medicine has proven that exercise is a cure for many health conditions. It is an undoubtedly important part in Sheffield Medical Centre’s CURE Method, a multi-faceted multi solution treatment plan that aims to help combat the overwhelming drug dependence in people suffering from chronic illnesses. Sheffield Medical centre prides itself in finding a unique approach to curing pain.

Sheffield Medical Centre’s Rehabilitation Gym a comfortable and enjoyable environment breaking the stereotype that going to the gym is an activity for the strong and youthful.
With the average age being 67.6, participants feel right at home in the centre without fear of judgement from others. The staff are trained to help and encourage the participants to lead an active lifestyle, despite their age and restrictive medical conditions.
The numbers to prove it
In the past ten years, the centre has seen 597 members come through its doors, with the eldest being 96. The largest age group is 71-80, with 172 members of that age coming in to exercise regularly. The centre prides itself on its inclusivity, and members can often be found saying that this gym is their centre of socialising, an excuse to meet up with friends and break a sweat.
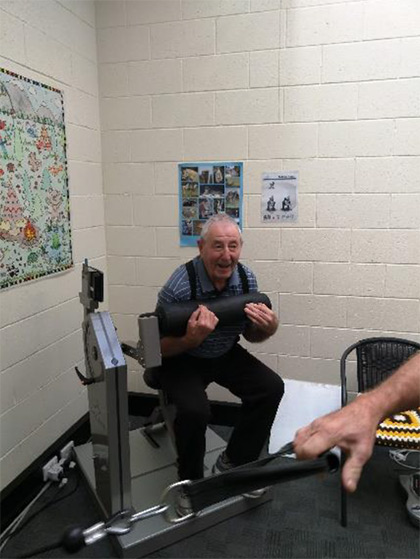
The gym shows no discrimination, and members are welcome in any shape or form. Several members suffer from various chronic conditions such as Diabetes and musculoskeletal problems. The staff are well-trained and are there supervising throughout the entire day, helping the members to reach their potential. The machines are gentle enough for even the most inexperienced of members, with weights going up in as little as 100g increments, to make the experience as pleasant as possible.
Average age – 67.6
Eldest – 96
Some more statistics:

| Age of Residents | Number of members |
| 19-30 | 2 |
| 31-40 | 7 |
| 41-50 | 93 |
| 51-60 | 68 |
| 61-70 | 128 |
| 71-80 | 172 |
| 81-90 | 90 |
| 90+ | 17 |
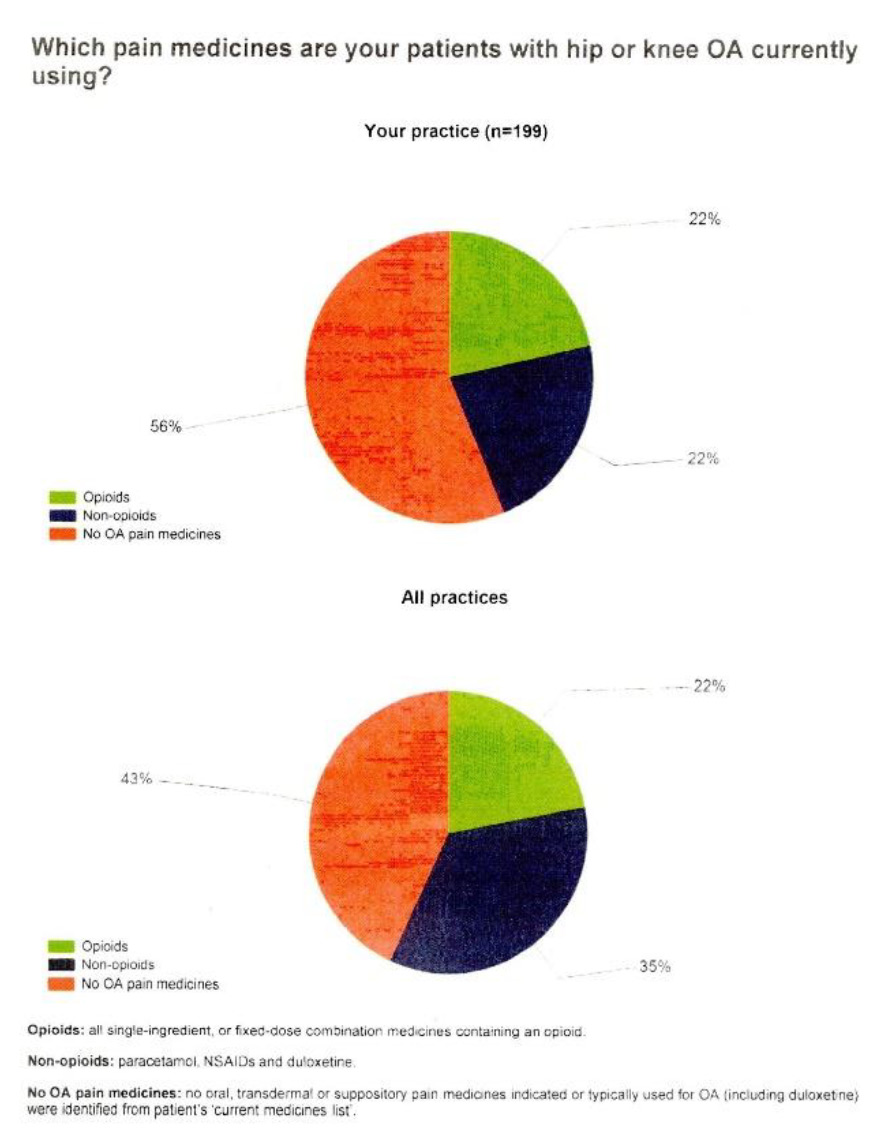
The result of our approach could be clearly seeing on the comparison graphs from NPS data. As we noticed, the use of Non-opioid medications for the management of the hip and knee OA 13% less than in other practices (22% in Sheffield Medical Centre against 35% in other practices).We also have to notice, that age of the patients visiting Sheffield is higher.
Age profile of your patients 1 July 2018 to 30 June 2019
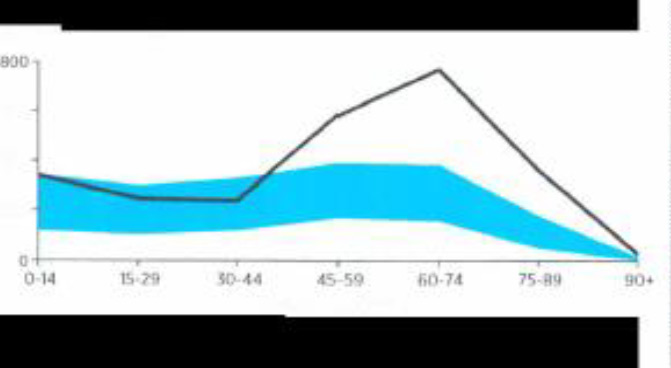
The black line represents the age profile of your patients.
The shaded area lies between the 25th and 75th percentile for GPs in your RA. *Data values are outside the range of the graph
If you would like more information on how to participate and be a part of this unique gym, please contact Sheffield Medical Centre for more information.
*Due to the recent circumstances with COVID-19, we have had to post-pone our celebrations. However, all will be going ahead once the restrictions have lifted and celebrate our special gym.
Prescribing and dosing exercise in primary care
John W Orchard AM, MBBS, MD, PhD, FACSEP, FFSEM (UK), FACSM, Adjunct Professor, School of Public Health, University of Sydney, NSW. [email protected]
Abstract
Background Exercise prescription, while not traditionally part of the medical school curriculum or many advanced post-graduate training programs, is rapidly becoming an essential skill in primary care. Its importance relates to exercise being an effective evidence-based intervention for osteoarthritis, back pain, tendinopathy, some cancers, depression, diabetes and cardiovascular diseases.
Objective The aim of this article is to describe the basic principles of exercise prescription in the context of a primary care medical consultation, assisting general practitioners to manage cases without the need for referral. Understanding the basic principles is important, but it should not be presumed that exercise prescription is always straightforward.

Discussion A good mantra for exercise prescription is ‘move, monitor, modify’. Failure of basic exercise prescription does not necessarily mean that procedural or medication treatment is required, but instead second-line exercise prescription may be indicated. Although referral to an exercise-based practitioner is a useful option, exercise prescription should become embedded as part of primary care medical practice because of its reported effectiveness and minimal side effects when appropriately implemented.
For many years, exercise has been seen as a healthy lifestyle pursuit but not a central part of medicine. There are now many conditions, particularly chronic diseases, for which exercise needs to become a critical first-line medical treatment to follow evidence of effectiveness.1,2 These conditions include osteoarthritis, back pain, diabetes, cardiovascular disease, depression and cancer, including breast cancer.3,4 Such chronic diseases now account for one-third or more of the entire health budget in modern Western society,5 all of them being named as ‘health priorities’ in Australia and collectively representing a high proportion of a general practitioner’s (GP’s) caseload.6,7
Exercise is particularly important as the first-line treatment for osteoarthritis and back pain, as emerging evidence in favour of exercise has coincided with strong evidence that many of the traditional medical treatments are actually not helpful.8,9 Opioid prescription is now to be avoided as a management strategy for osteoarthritis and back pain because of the potential for addiction and other serious side effects in the long term.10 While non- steroidal anti-inflammatory drugs (NSAIDs) are still recommended as a treatment option for osteoarthritis and back pain, they confer a 30% increase in major cardiovascular events in users;11 therefore, they are unsuitable for patients who are in the high-risk group for a cardiovascular event. Some of the traditional surgical procedures in musculoskeletal medicine, such as knee arthroscopy for degenerative knee conditions12 and spinal fusion for chronic back pain associated with disc degeneration,13 have now also been downgraded as management options because of their inability to perform better than placebo or comparison treatment in randomised controlled trials.
This evidence has rapidly expanded in the past decade; therefore, many family practitioners may not have been taught how to best prescribe exercise during either their medical school or postgraduate training.14 Referral to an exercise physiologist, physiotherapist or sport and exercise medicine physician15 is an available option (Box 1), but the need to include exercise prescription as part of the management plan for such an array of conditions means that a basic skill set is now an important part of primary care.
Key concepts in exercise prescription. Exercise and all-cause mortality
Very strong cohort evidence from multiple studies shows that baseline exercise levels are highly predictive of all-cause mortality in both men and women,16,17 and are also predictive of cardiovascular disease18 and cancer.19,20 The correlation between exercise (at moderate levels or higher) and all-cause mortality is higher than the correlation between body weight and all-cause mortality.21–23 From a health outcomes viewpoint, it would therefore be beneficial to move away from a focus on body weight in favour of measuring physical activity. Although exercise is difficult to define and measure precisely when compared with body weight, body mass index (BMI) and other measures such as blood pressure, wearable step-counting technology (included in all late-model smartphones) makes accurate estimation of baseline exercise more simple than it previously was.24 Consumer wearables are rated as being accurate enough for self-monitoring but not yet the gold standard for research into physical activity.25
Conclusion
Exercise prescription, although not part of the standard medical school curriculum, is now an essential skill in primary care. Exercise is an evidence-based treatment for osteoarthritis, back pain, tendinopathy, some cancers, depression, diabetes and cardiovascular diseases. It requires more than rudimentary understanding to successfully implement, as patients can become disheartened by temporary pain flare-ups. The need for medicinal and procedural treatment for many conditions can be reduced if proficiency in exercise prescription is developed.
There is an acknowledge that the article’s abstract is reproduced with permission from the RACGP Aust Fam Physician
2020;49(4):182–86.
Full article available at www1.racgp.org.au/ajgp/2020/april/prescribing-and-dosing-exercise-in-primary-care
Fat Cavitation and Skin Tightening as part of the weight management problem.
Article by Jasmine Ung
Contouring by Jaz
Epping, Victoria
One of the many ways to boost the results of exercise and healthy living is through
Ultrasound Fat Cavitation and Radio Frequency Skin Tightening. Many people – despite the fact that they are consistent in their training – may lose motivation throughout the process as they hit various plateaus. Though the procedure itself may not produce instant results, with the help of some pre-requisites, such as a healthy diet and consistent exercise, fat cavitation is able to finally get rid of that stubborn fat that just will not disappear or any cellulite which just will not reduce. The question then lies, what exactly is fat cavitation?
Ultrasound Fat Cavitation is a non-invasive body contouring treatment which uses low frequency ultrasound waves to flush fat from the body. Fat cavitation should not be treated as a weight loss solution, but rather as an amplifier. If exercise was the engine, fat cavitation is the turbo.



Before we understand the procedure of fat cavitation, we must first learn that there two types of fat: subcutaneous fat and visceral fat. Subcutaneous fat tissue sits in front of the muscle beneath the skin. It is the pinch-able, the grab-able fat on your body. Visceral fat is the deep internal fat, which sits behind the muscle wall, though it should not be confused as a bad thing, as this fat plays a role in insulating and
protecting your internal organs. However, excessive amounts of Visceral fat can cause serious problems in your health. Fat Cavitation targets the Subcutaneous fat on your body, to get rid of “love handles” or that double chin that just won’t go away.
So how exactly does the procedure work?
Firstly, ultrasound gel is applied to the target area, followed by the therapist operating a hand piece which emits low frequency sound waves. which then produces tiny bubbles within the fat cells, disrupting the outer membrane, which causes tiny collections of fat to be expelled through the body’s lymphatic system. Fat cavitation does, however, have its pre-requisites, as well as some limitations.
Fat cavitation should not be treated as an “instant” weight loss solution, but rather be used as an amplifier to boost the results of exercise and a healthy diet. The treatment is also more effective with frequent sessions (recommended weekly), as the procedure breaks down the stubborn fat cells over time. After 6-12 treatments, optimal results are expected to be seen.
Drinking at least two litres of water before and after the fat cavitation treatment is considered a prerequisite to facilitate the elimination of broken-down fat. In
conjunction with Fat Cavitation, another procedure known as Radio Frequency Skin Tightening is used. RF Skin Tightening is the procedure of producing energy to heat the skin with the purpose of stimulating the production of collagen and elastin within the skin, causing immediate contraction. This contraction results in the tightening of skin layers which creates smoother, healthier, and younger looking skin. RF Skin tightening also has other benefits, such as improving the blood and lymphatic flow, better oxygen supply and greater toxin clearance to further reduce the effects of ageing. Though both Fat Cavitation and & RF Skin Tightening are separate procedures, there are ultrasound machines which are able to produce both treatments in the one handpiece, so there would not be a need to have two separate sessions done. However, if you were to opt for just the one treatment, this is also possible.
In conclusion, if you’ve felt like you’ve hit a plateau in your weight loss and simply cannot get rid of stubborn fat, despite your best efforts, then Fat Cavitation and RF Skin Tightening might be worth a shot, and might just be the answer you’ve been looking for.
Case study.
Dr. Serguei Kisselev
D.C., 85 y.o lady with multiple medical problems:
- Bilateral Knee OA, severely negatively affecting her sleep, walking and other activities of daily living
- Cystocelle and rectocelle, associated with incontinence – both urinary and faecal and experienced constant pelvic pain. Pelvic floor repair – 2014 with only minimal relief of the symptoms
- Asthma
- Hypertension, Congestive heart failure
- Oesophageal dysmotility
In 2012, after discussion about her ongoing health and social problems and possible scenarios of their further progression, she was explained the benefits and recommended “CURE” program.
She started to visit Rehabilitation exercise program of the Sheffield Medical Centre at age of 78.
Before she started exercised she had an introductory course of the “muscle retraining” electrostimulation therapy with “Russian Current” – 10 sessions, twice a week, 20 minutes each areas – with aim to improve muscles strength of the body core and proximal legs and to avoid or minimise possible negative muscle pain impact associated with initiating of exercises.
She has been visiting Rehabilitation Exercise classes once or twice a week for 90 – 120 minutes each time.
During all this time she also has had several courses of Prolotherapy, Photobiomodulation (Former named as Low Level Laser Therapy) on her legs/knees and lumbar area to manage the aggravation of the pain in low back and knees and hip joints.
She also noticed that her pelvic pain become less severe. From 2017 every 6-8 months she has had courses of combined PBM/LLLT + TENS(“Russian” current ) pelvic floor muscle retraining. As a result, her pelvic pain and continence problems much eased and have only minimal impact on her every day’s life. He ability to walk, look after herself and to be independent in most aspects of her life much improved and stable over the last eight years.
Her own impression is
D.C: I’ve have had bad arthritis in my knees, and that has… with all the treatment that I’ve had, that has helped them. Sinus and prolapse, also. And so I’ve had laser treatment, and so I’ve found that the gym has been wonderful.
Doctor: So how do you feel today?
D.C: I feel well
Doctor: So do you think what we’ve done in our clinic is helping?
D.C: Absolutely.
Australian study finds resistance training improves cognitive function in older adults
By Jane Lewis
Medicine Today 2016; 17(12):10

A randomised controlled trial, led by researchers at the University of Sydney and published in the Journal of the American Geriatrics Society, has found that high- intensity progressive resistance training (PRT) can significantly improve cognitive function in older adults with mild cognitive impairment (MCI), and that strength gains mediate these cognitive benefits.
‘Although most research to date has focused on aerobic exercise such as brisk walking, there is emerging evidence that resistance training – strength training or weight lifting – may be equally if not more powerful in terms of brain health and cognitive function,’ Professor Maria Fiatarone Singh, geriatrician at the Sydney Medical School, University of Sydney, and senior author on the paper, told Medicine Today. The research was based on results of the SMART (Study of Mental and Resistance Training) trial, first published in 2014, which demonstrated that six months of PRT (two days per week) significantly improved global cognitive function in community-dwelling adults with MCI (n=100; age >55 years), as measured by tests including the Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog). In addition to its effects on cognitive function, PRT also significantly increased upper, lower and whole body strength, and percent change in VO2 peak (8.0%), compared with sham exercise.
The current study set out to further investigate the effect of PRT, finding that that improvements in strength, rather than aerobic capacity, mediated the improvements in ADAS-Cog and global domain. A near significant mediating effect of strength on executive function was observed, with no effect observed on memory domain.
‘Although we don’t yet know how it works, there is evidence that individuals who gain the most strength after weight lifting exercise also enjoy the most cognitive benefits,’ explained Professor Fiatarone Singh. ‘It may be that a common factor, such as a growth factor that is good for both muscle and neural tissue, explains this association. More research is in progress to identify the molecular biomarkers and pathways involved so that optimum interventions can be designed and tested.’
Strength training has many other benefits for older adults – helping to address sarcopenia, osteoporosis, arthritis, diabetes, neurodegenerative diseases and many other conditions, in ways in which aerobic exercise does not – and can be ‘far more feasible’ than aerobic exercise in those with severe mobility impairment, arthritis or low thresholds for ischaemia or dyspnoea, she added.
J Am Geriatr Soc 2016; doi: 10.1111/jgs.14542.
Medicine Today 2016; 17(12): 10 Link at: https://medicinetoday.com.au/in-brief/australian-study-finds-resistance-training-improves-cognitive-function-older-adults
“Physiotherapy and the gym”
Sarah Lyons, Physiotherapist
Physiotherapists can treat a wide variety of musculoskeletal, neurological and cardiovascular conditions. Physiotherapy treatment may involve therapeutic exercise to improve strength, range of motion and endurance and to correct postural and muscle imbalance. This in combination with local soft tissue therapies, joint mobilisation and manipulation to relieve stiffness and pain.
Having access to a fully equipped and manned gym onsite means your physiotherapist can collaborate with you as the patient and staff to provide guidance through a personally tailored strength and conditioning program. It is no doubt that regular exercise can benefit your health, mind and body. Not only does it boost your energy, increase lean muscle mass, decrease your risk for certain health conditions. It can help you manage your weight; it improves your mood and can significantly reduce the chances of repeat injury and trauma. Your program can be easily modified and adjusted through a follow up visit with the physiotherapist or discussion with the onsite personal trainer.”
Sarah Lyons, who owns a physiotherapy clinic in Launceston and a physiotherapist herself, also attends to the patients in our clinics across North/North West of Tasmania. Sarah has adopted our CURE approach.
You can find Sarah’s clinics details below:
Web: http://riversidephysiotherapy.com/
Facebook: https://www.facebook.com/Riverside-Physiotherapy-1657130881073954/

Would you like to be a part of the CURE Method?
Roman Kisselev – Manager of the Your Health Connect Group
Website: https://tasgpjobs.com.au/
Facebook: https://www.facebook.com/tasgpjobs/
Instagram: https://www.instagram.com/tasgpjobs/?hl=en